The Significant Impact of Oestrogen (or lack of)!
Menopause is a natural stage of life that all women experience, yet many are surprised by just how much it can impact it has on their body, and how suddenly! As physiotherapists, we often see women in their 40s, 50s and beyond struggling with new aches, stiffness, pains and injuries that seem to appear “out of nowhere.” There is no doubt that hormonal changes during menopause play a significant role in musculoskeletal health.
What Happens to Oestrogen During Menopause?
Menopause marks the end of menstruation, and typically occurs between ages 45 and 55. The main hormonal change during menopause is a significant drop in oestrogen which is a hormone produced primarily by the ovaries. Oestrogen plays a crucial role in reproduction, AND in the health of many body systems.
Whenever oestrogen levels decline, the body undergoes a range of changes, particularly in the musculoskeletal system. Understanding the role of oestrogen helps us explain why menopause can become such a time for new and unusual pains.
How A Lack Of Oestrogen Impacts Our Tissues
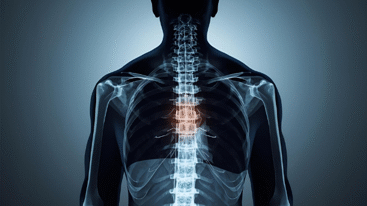
Oestrogen and Bone Health
Bone is one of the most metabolically active tissues in our body – every second of our day bone cells are being broken down (resorption of old bone) and replaced with new bone cells (formation of new bone). Oestrogen plays a critical role in balancing this bone remodelling, and ensuring the resorption is matched by new formation.
Key effects of oestrogen on bone:
- Oestrogen controls bone resorption: OsteoClasts are the cells that break down old bone tissue. Oestrogen suppresses the activity and lifespan of osteoclasts so less oestrogen means more osteoclast (breakdown) activity, leading to accelerated bone loss.
- Oestrogen promotes bone formation: Oestrogen also supports the function of osteoBlasts, the cells responsible for building new bone. So less oestrogen means less new bone formation.
This oestrogen deficiency that occurs during and after menopause causes a rapid imbalance: accelerated bone resorption and breakdown outpaces new bone formation, resulting in a net loss of bone.
This puts menopausal women at greater risk of:
- Osteopenia (early-stage bone loss)
- Osteoporosis (more severe bone thinning that increases fracture risk)
In fact, women can lose up to 20% of their bone density in the 5–7 years after menopause. This is why fractures from simple falls become more common in peri/menopausal women.
Oestrogen and Tendon Health
Oestrogen also influences the structure and function of tendons, the connective tissues that attach muscle to bone.
Key effects of oestrogen on tendon:
- Collagen regulation: The key structure that makes up the strength, resilience, and elasticity of our tendons is Type 1 collagen. Oestrogen promotes collagen synthesis and turnover, and it also helps maintain the ability of our tendons to stretch and recoil efficiently.
- Hydration and vascularity: Oestrogen supports tendon hydration and blood flow, essential for tendon health and repair.
What happens to tendons after menopause:
- Lower oestrogen levels can lead to:
- Reduced collagen synthesis, weakening tendon structure
- Decreased tendon elasticity, increasing stiffness
- Higher risk of tendon pain or injury, especially in the shoulder, gluteal tendons, achilles, and plantar fascia
Oestrogen and Muscle Health
Muscles are also affected by hormonal changes. With lower oestrogen levels, women may experience:
- Reduced muscle mass and strength
- Slower muscle recovery after exercise or injury
- Increased muscle stiffness or joint pain
Other Health Effects of Menopause
In addition to bone, tendon, and muscle changes, menopause also affects:
- Metabolism: leading to weight gain, especially around the abdomen
- Sleep quality: due to night sweats or insomnia
- Mood: increased risk of anxiety or depression
- Cardiovascular health: oestrogen helps protect heart and blood vessels, so heart disease risk may rise post-menopause
All of these factors can influence your ability or motivation to stay physically active—which in turn affects muscle and bone health. A vicious cycle!
How Can You Protect Your Body During Menopause?
The good news is there’s a lot you can do to reduce the impact of menopause on your musculoskeletal system. Here’s what we recommend from a physiotherapy/musculo-skeletal perspective:
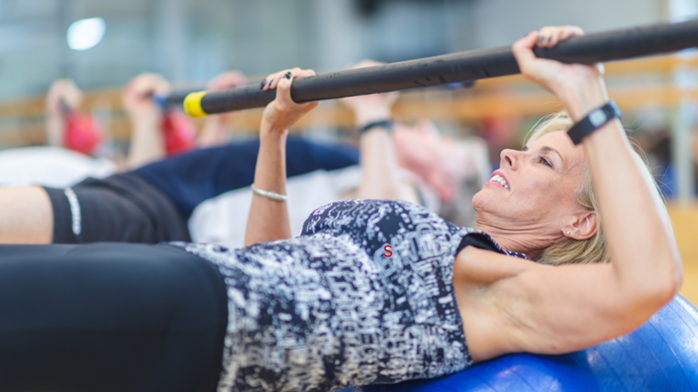
Start (or Maintain) a Strength Training Program
Resistance training is one of the best ways to:
- Preserve and build muscle mass and tendon resilience
- Strengthen bones
- Improve balance and reduce fall risk
This doesn’t mean you have to lift heavy weights in a gym—simple bodyweight exercises, resistance bands, or light dumbbells can be very effective when done regularly.
Weight-Bearing Activities
Exercise such as walking, hiking, and Pilates that puts gentle stress on bones helps them stay strong. However, we know that variation is important with weight bearing exercises – going for the same distance/pace/route of walk every day may not “excite” your bone cells enough to create the required stimulus for change – adding different surfaces, speeds, stairs are some ways to add variation to your walking program.
Nutrition Matters
Ensure you’re getting enough:
- Calcium (for bones): found in dairy, leafy greens, almonds
- Vitamin D (for calcium absorption): from sunlight and supplements if needed
- Protein (for muscles): lean meats, fish, legumes, dairy, nuts
Stay Consistent with Physiotherapy
If you’re noticing aches, pains, balance issues, or weakness, don’t wait for things to worsen. Physiotherapy can:
- Help manage tendon and joint pain
- Provide targeted strength and mobility exercises
- Monitor bone health risks
- Keep you moving confidently and safely
Final Message
Oestrogen is not just a reproductive hormone—it’s a key player in maintaining the integrity of bone, tendon and muscle tissue. When oestrogen declines during menopause:
- Bones become more fragile due to increased resorption and reduced formation.
- Tendons become stiffer, less resilient, and more prone to overload or degeneration.
This is why strength training, targeted loading of tendons, and early physiotherapy intervention are so important for menopausal and postmenopausal women. Combined with good sleep hygiene, optimal nutrition (and HRT as needed) you really can make a difference to these midlife pains!
Anthony Lance SSPC Physiotherapist References available on request.
You might like these other resources
Is This the No. 1 Mistake a Runner Makes?
19 January 2026
The Hidden Driver Of Pain – Why Thoughts & Beliefs Matter!
24 December 2025
Why Do My Joints Ache In Cold Weather?
11 June 2025